This weekend I am live blogging from the Students With Diabetes Leadership Conference 2014. Keep checking back here for updates all weekend, and follow along on Twitter at #SWD2014 as the weekend picks up steam.

The Leadership Conference is a preliminary session of the Students With Diabetes 2014 National Conference for students WITH diabetes who have earned and have been awarded a summer internship with diabetes companies, like Novo Nordisk and Tandem.
Friday, June 6, 2014 – SWD2014 Leadership Confernce
8:15am – About eight students with diabetes are awake and downstairs early for breakfast this morning. More trickling in from upstairs. The Heat lost 110-95 last night, so some of us are more excited about having stayed up so late watching the game than others. Like Reagan from Texas. He is a happy San Antonio Spurs fan this morning. Still…go Heat! Where’s my coffee?
9:00am – Nicole Johnson welcomes the student leaders to the SWD2014 Leadership Conference. About 20 students with diabetes in the room, ready to discuss and engage each other and today’s leadership speakers who will be sharing incredibly valuable insight from the business of diabetes, health, communications, and so much more.
9:15am – Donna Petersen, Dean of the University of South Florida College of Public Health, is on stage to talk about how we define “health” in our society, and what we can do as leaders to connect the dots and inspire change in public health.
9:55am – Talking about challenges in public health, misconceptions, insurance policies, and brainstorming ways to change the systems that we all have to deal with, diabetes and otherwise. Cost and access to healthcare (in all ways, shapes, and forms) is a big theme in this discussion.
10:00am – Project time. Next we’re going to work together to determine each of our personal values. Values are the guiding principles that inform our directions, our choices, and our actions. This project will lead to a vision and an action plan for where the student leaders in this room are headed next. Exciting!
10:20am – Around the room, everyone has made a list of 20 values, and have whittled it down to 3. Trying to get focused here at SWD2014! In related news, a paper shredder has been requested to dispose of all evidence of values that didn’t make the value cut. This is proving to be a very difficult and telling exercise. And incriminating. Mostly incriminating.
10:25am – Break time. Low station has been found. I’m totally eating Spicy Nacho Doritos because I’m low. Honest. It’s for my diabeetus!

10:40am – Rick Gallegos, CEO of Dale Carnegie training in the Tampa area, to talk to us now about how you present yourself. Asking some questions about what people think about in presenting themselves. Answers include being dressed properly, being prepared, being able to speak publicly and communicate well. Fear of public speaking is greater than fear of death by fire, and fear of death by drowning (according to Rick…although if he had watched last week’s Game of Thrones, that list might be different. Popped like a grape!)
10:45am – Attitude is everything. “Of course I can do that!” And repeat. Hi-fives make for good reinforcement of the “Of course I can do that!” ‘tude.
10:55am – I met a nice lady at SWD2014 named Lauren. She met a dude name Martina. There is a story there. Something about using and not using middle names and initials, and how I’m sitting next to a complete stranger! (Lauren Nicole Johnson and Martin Allen Wood – Someone should probably separate us before we get in trouble for giggling too loud and being disruptive.)
11:00am – Learning how to associate names with a story when meeting people. From this point forward, everyone I meet is getting a superhero backstory. You’re welcome.
11:15am – Listening to Q&A among students. Getting to know each other. The conversation is absolutely fascinating, and the students with diabetes in this group are so interesting. Enjoy hearing how different (and not) we all are, and finding what we have in common (beyond just diabetes). Like how everyone here is a huge Heat fan! (Maybe not entirely accurate, but can we all just have that in common for the sake of this conversation?)
11:30am – Wrapping up with Rick Gallegos. Next, I’m up, talking about leadership and professionalism and what people look for in good employees, and applying that to both a career and your diabetes.
11:40am – Nicole here. Martin Wood is now speaking – teaching about real life with diabetes. “Been there done that and have the tattoo.” Love this guy!
11:45am – “Be memorable. Every experience you have is an opportunity to connect with someone else, diabetes or otherwise.”
11:50am – “There is no shame in sharing about T1D with colleagues. You judge yourself more than others judge you.”
11:55am – “You are not going to be successful if you hide who you are. Don’t discount your value.” – awesome speaker!
11:55am – Someone asked, “What is the one thing that you consider your biggest accomplishment?” Martin, “I’m still here. That is my greatest accomplishment. Despite diabetes, professional setbacks, personal setbacks, and everything that the world has thrown at me in my 35 years, good, bad, and otherwise, I am still here.”
12:00pm – Lunch break. Salad (healthy), half a sandwich (healthy), tomato soup (healthy), peanut butter cookie (totally healthy). Peanut butter is used to make peanut butter cookies, and peanut butter has protein in it, which helps maintain blood sugar levels, which means more peanut butter cookies. Science.
12:30pm – Mind blown during lunch today. Realize that my friend Gilles and I go WAY back. Neither of us realized the connection until today. Holy cow! (I’ll tell the story in a follow-up post, and put the link here. It’s a story worthy of its own blog post.)
1:15pm – Tom Boyer, the Government Affairs (and most knowledgeable person in the nation) person for Novo Nordisk. He is here to talk about government policy + diabetes = diabetes policy in government, and advocating on The Hill for people with diabetes.
1:30pm – Tom is talking about professionalism on the job. Dress appropriately, professionally. Don’t check your phone while talking and interviewing people. Don’t use your computer when a pen and paper will suffice (unless it’s your job, that’s different…don’t get carried away people). Focus on what is most important, which is the person you are talking to, and what the conversation is about.
1:50 – Since the SWD Leadership Conference is helping to prepare the students with diabetes for their summer internships in the diabetes biz, Tom is shining a light on other people who started with a job as an intern. — Brian Williams, Brooke Shields, Tom Hanks, Bill Gates, Lauren Conrad, Conan O’Brien, John Krasinski, Jodie Foster, Patrick Ewing, Anderson Cooper, Betsey Johnson (even if she did go bankrupt, she made a lot of money going bankrupt…so…successful), Steven Spielberg, Tom Ford, Roger Goodell, P. Diddy, Oprah Winfrey, Steve Jobs. Who says this blog isn’t educational?
2:10pm – “Show up early, work late. If you show up late and leave early, it’s going to be game over for you quickly.” – Tom Boyer
2:15pm – “In business, you have to manage people, and you have to manage money. Those are the two most important components that being successful in business comes down to.” – Tom Boyer
2:15pm – Activity time! Developing a personal Elevator Speech.
1. Make them care.
2. Make it easy to join.
3. Leave them wanting more.
4. Have a call to action.
5. Be natural.
6. Test yourself.
2:30pm – You never know when the opportunity to share your personal elevator speech will present itself. Define it. Refine it. Know it. Make it memorable. Make it actionable. Be specific about what you need next, and how the person you are talking to can help you to make it happen.
2:40pm – Imagine you have 60 seconds to nail your elevator speech. Every word is important. Every word has a purpose. Know what you are selling, intimately. Know what you are asking for, specifically, and always be closing (ABC people: Always Be Closing).
3:00pm – Wrapping up the Leadership Conference. This is the only program that the pharmaceutical industry has to identify interns with Type 1 diabetes. Pretty cool, connecting opportunities for people with diabetes to work in diabetes. The big SWD2014 conference kicks off in a little while. For now, a few hours break while we shift gears.
Saturday, June 7, 2014 – SWD2014 National Conference
After a fantastic and entertaining evening last night with actor, comedian, and diabetes advocate Jim Turner, followed by a dance party and socializing galore (like you do at a diabetes conference), everyone seems to have had a good night sleep (or a good hour or two of sleep), and we’re back for Day 2 of SWD2014. Here we go! Where’s my coffee?
9:15am – After a Zumba workout this morning and a nice healthy breakfast (eggs, cereal, coffee, a little more coffee, and there was also some coffee), Nicole Johnson is introducing our first speaker this morning, Mr. Mike Lawson from the Diabetes Hands Foundation and TuDiabetes social network, to share with us Diabetes Funnies. Mike is a graphic designer and also creates YouTube videos, and is a leading voice in the diabetes online community (DOC).

9:25am – Mike is sharing his stories of living with diabetes, and how he uses social media near constantly to laugh and live with diabetes. Solutions are sometimes right where we least expect them. Mike shares on social media a lot, and uses social media to help him and his diabetes.
9:30am – Seeing videos of Mike and Ginger Viera. If you don’t know Ginger (or would like to, because she’s ridiculously awesome as well), check her out on Twitter at @GingerVieira. Here is their video “Livin’ With Diabetes” on YouTube.
9:35am – Activity time! Questions that are often asked of people with diabetes, and the response has to be in sign language. But no obscene gestures, because this is a family show. Mostly.
9:45am – Now we’re creating diabetes meme’s from “Success Kid” and “Grumpy Cat” and “Not Sure Fry.”


10:00am – Break time, then in 15 minutes we are headed to breakout sessions. We’ve got discussions happening on Diabetes in the Workplace, The Insurance Zone, Pregnancy, Relationships (and everything that goes along with them), Diabetes and Exercise, and even Type 3’s (people who love and are a part of the lives of people with diabetes).
10:15am – In the breakout session with Tom Boyer from Novo Nordisk, talking about diabetes in the workplace and health insurance in the United States. Sounds like there are a lot of questions in the way of concerns when applying for jobs, seeking insurance and a fulfilling career at the same time, patient advocacy, and coworkers that don’t understand diabetes, among other issues.
10:20am – Tom is a big advocate for reading the newspaper every single day. He also shared that advice with our interns in the Leadership Conference yesterday. He starts every morning reading the newspaper, and finding out what is going on in the world. It’s one of the easiest things you can do to be ahead of the curve compared to your peers, and also to be well-informed so that you can make decisions based on current and more accurate information. This WILL lead to a better financial situation over the long term. (Do you do this? I’m a librarian, and I’m ashamed to say that I don’t even do this, though I do try and keep up via the internet. What newspaper(s) do you read?)
10:25am – “Find a job that has reasonable benefits.” Reasonable is defined as a robust level of coverage for YOUR needs (because individual and family needs vary). Also consider retirement options and the company’s match program (many companies will match your retirement investment up to a certain %). Also consider how long it will take before you are vested with your retirement, and if you will be at the job long enough to receive the benefit.
10:30am – “The greatest thing that has helped with health insurance in the last 30 years is the Affordable Care Act. Whether you like it or not, it’s the truth. The governor’s who are holding out are taking advantage of people with chronic conditions, and we are and should be extremely upset that the holdouts are threatening and taking advantage of us.” — Tom Boyer
10:31am – Q. How do we help to try and improve the situation with the governors and state legislatures of states that are holding out? — A. States are choosing to pass up millions of dollars from the federal government to withhold benefits to certain classes of people. Show up at town hall meetings and hold these representatives accountable and take them to task on the needs of people with diabetes and other chronic conditions. Letters no longer work effectively to contact members of the legislature due to security reasons, making it nearly impossible to interact with them via mail.
10:35am – Legislation in California, AB 1893, was proposed and seriously considered and debated to force people with diabetes to buy a sharps container for every 50 needles purchased (syringes, lancets, etc.). Some companies were in favor of this. Novo Nordisk, who was strongly against it, brought in advocates from the diabetes patient community to push back on the legislation, taking representatives to task, and successfully defended patient rights and helped kill the bill. Turns out the bill was backed by representatives who were benefiting from funding from companies who would have profited from the mandatory sales of sharp containers. Capitalism at its finest. Know who you are voting for people, regardless of what side of the aisle they are on.
10:40am – Politics have identified patients as the weak spot for fundraising and giving. In some states, they can accept corporate donations (under the table, soft money, not reportable), which inherently influences legislation.
10:45am – ADA and JDRF have not weighed in the extra $1,000 per year cost of the sharps container legislation. Students With Diabetes, American Association of Diabetes Educators, Diabetes Hands Foundation, the Pediatric Endocrine Society, and others are speaking up. Hold the people you partner with to task, and strongly urge them to advocate on your behalf.
10:50am – Rights in the workplace are always a challenge. Employers often mandate what employees can and cannot get covered by health insurance. In the case of denials, there is an appeal process, but it often requires data and support from your endocrinologist and healthcare providers. Continuous glucose monitors (CGM) and sensors are still challenging because many insurance companies consider CGM to be a “luxury item” rather than a necessity. Show them the data, your data, and take them to task. For pump hardware and supplies, refer to Medicare Plan B, and hammer the insurance company on it. Insurance companies are required to cover pumps and pump supplies, by law.
11:00am – Florida’s governor (Rick Scott) rewrote the insurance laws covering people in the state of Florida when he took office, essentially providing employers a way to not have to provide full insurance coverage to people with chronic conditions, and effectively making it much more difficult (if not impossible, in some cases) to get necessary prescriptions and supplies covered. — (Florida people with diabetes, remember this when you vote this Fall, and carefully consider whether you want to support someone to make decisions on your behalf that doesn’t support you in return. This has nothing to do with partisanship, and has everything to do with staying focused on what YOU need as a person with diabetes.)
11:02am – Employers are not allowed to ask if you have diabetes, or even dance around the topic. You are not required to disclose that you have diabetes at the workplace.
11:03am – Massachusetts has the most sophisticated health system in the United States of America, with the best doctors on the planet (Joslin, Beth Israel, etc.).
11:04am – In California, there is a purchasing pool that allows people to get health insurance no matter where they work or live in the state.
11:06am – In Texas, the rate of diabetes is skyrocketing (33% increase in T1 in children in the last 10 years). Diabetes is the #2 reason for hospital admissions in Texas. The best way to get diabetes health coverage in Texas is to be a woman with diabetes and pregnant.
11:08am – You are going to see a lot of migration out of states that do not offer proper health insurance coverage, or make it extremely difficult to get it, to states that are more accommodating to people and their healthcare needs.
11:09am – In Florida, the governor does not believe that healthcare reform is a priority. As a result, coverage is lacking. Students with diabetes can stay on their parents policy until they are 25 (or is it 26?), and are encouraged to stay on those plans and pay the discounted premium until the last possible date.
11:10am – The work that you will have to do to find health insurance in states whose leaders do not support the Affordable Care Act, like Florida, Texas, and South Carolina, is much greater than states who have embraced the federal mandates, like California and Massachusetts.
11:15am – 1. Keep your debt manageable as you progress and start your careers. 2. Live in a state that provides reasonable health coverage.
11:30am – Brian Fee, who has had Type 1 diabetes for 10 years, is an athlete and regular participant in marathons, duathlons, and cycling races. In this breakout session on Diabetes and Exercise, we’re talking about how to train and workout with diabetes.
11:33am – There are a few important factors when planning your exercise and training.
1. Set realistic goals.
2. Find a training program.
3. Prepare mentally.
4. Find supplements and equipment that fits and works for you.
5. Find help amongst friends.
6. Training should be informative and fun.
11:35am – At diagnosis, Brian, like many of us, was reminded over and over about what he could not do with diabetes. This inspired him to defy the odds and discover what he COULD do with diabetes.
11:40am – Managing BG levels while exercising is important for many reasons, including endurance, performance, and also safety. Important to test before, during, and after working out so that you can get baselines and know what is going on.
11:42am – Keep a journal so that you can track your progress. Track lows, highs, heart rate, and how you feel at the time (strong, weak, like you can do more, etc.)
11:45am – Brian is sharing some great advice about nutrition, hydrating, and fueling your body during exercise. Also stressing the important of safety, letting someone know what your plans are, where you will be when exercising (such as if you’re going on a long bike ride), and carrying your personal information on your body somewhere. Recommend Road ID, who makes bracelets and other accessories for identification and personal information.
11:49am – Sometimes the chains that prevent us from being free are more mental than physical.
11:55am – Matt O’Brien is a personal trainer with Triumph Functional Fitness. His brother has Type 1 diabetes, which was his first exposure to the world to Type 1 diabetes. He now has multiple clients with Type 1 diabetes, and also many more with Type 2 diabetes.
11:57am – You can pick up Matt’s book, The Magic Pill, on Amazon.com.
12:05pm – “Failure to plan is planning to fail.” Planning is key to getting the most out of exercise.
12:20pm – Lunch break. Then we’re going to hear all about the bionic pancreas (I am SO excited!).
1:45pm – Very excited about this presentation! Dr. Ed Damiano from Boston University is here to present “Making diabetes management disappear: A bionic pancreas for one and all.” – I want this…really, really bad.
1:48pm – Imagine two insulin pumps, one with insulin and one with glucagon, and wearing them together (with some fancy computer programming) to prevent blood sugar from going too high or low.
1:49pm – The bionic pancreas uses CGM to take the management burden of diabetes off of your shoulders. It will still require some maintenance activities (calibration fingerpricks for the CGM, change insets, refill reservoirs…same as today), but will be able to adjust itself to changes of insulin requirements. The programming makes it smart, and it learns your individual insulin needs over time.
1:50pm – The bionic pancreas is a device that will adjust automatically for ever-changing insulin needs (when you eat too much, exercise too much, get sick, whatever the case may be).
1:53pm – The inspiration for the creation of the bionic pancreas was David, Ed Damiano’s son, who was diagnosed with Type 1 diabetes when he was a child. The idea is to find a way to decrease the burden of diabetes on daily living. The goal with this project is not to find a cure. It’s to make living with Type 1 diabetes better.
1:56pm – Diabetes is absolutely relentless, and it is on you 24/7. We have the technology. We can make life with diabetes better by reducing the burden so that you don’t have to focus on diabetes so hard, and can focus on other things.
2:00pm – Started bionic pancreas research with trials on pigs, who will eat anything (true story), and whose pathology resembled the pathology of a human being with diabetes. The pigs, like humans, also liked McDonald’s. (I’m loving it! And I want the bionic pancreas!)
2:02pm – Studies for the bionic pancreas led to testing various CGM devices to determine if CGM could be relied upon to make insulin dosing decisions, and prevent both hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar). The evolution of the research done over the past 10 years have led to better and better algorithms to manage blood glucose levels.
2:05pm – Recent studies only relied on weight to begin calibration, and 18 hours later the bionic pancreas algorithm figures out what your insulin needs are. Depending on insulin sensitivity, it may even take less time (if you’re more sensitive to insulin). In less than a day, the technology figures out how much insulin you need around the clock. Around the freaking clock! What?! I want this so bad right now! (This is me, on the verge of pitching a fit.)
2:10pm – Submitted dual pumps and iPhone (as the computer, locked out of apps and functionality not related to the trial) for testing and human trials to the FDA on October 31, 2012. 30 days later, on Ed Damiano’s birthday, they received approval to proceed with the trial.
2:11pm – Over the next year, the 2nd summer trials are taking place at Camp Clara Barton and Joslin Diabetes Camp, as well as a multi-center study. The multi-center study will be adults who wear the device around the clock, at home, and go about their normal lives for a few days without having to deal with diabetes decisions (again, outside of minimal maintenance). Expect both of these trials to go through January 2015.
2:19pm – Watching Ed Damiano demo the bionic pancreas technology, on an iPhone, with a Dexcom G4 custom attached. I’m having a hard time typing because I’m close to speechless.
2:22pm – Ed is showing his own CGM reading, and how even someone WITHOUT Type 1 diabetes spikes after food. To everyone in this room, he stressed not to beat ourselves up and stress out because we have a post-meal spike in blood sugar. It’s normal. IT IS NORMAL! A fully functional pancreas and immune system does not result in a flat blood sugar trend. It requires and should be corrected. That is NORMAL. It’s also normal.
2:26pm – Software makes it easy to teach the system how to define “usual” or “typical” when it comes to breakfast, lunch, or dinner. It gets away from defining diabetes based on hard data numbers that aren’t flexible, and are also sometimes unknown (like when you go out to a restaurant to eat and you have no stinking idea how many carbohydrates were in that plate full of deliciousness that you just stuffed into your face hole).
2:31pm – The bionic pancreas will also work without CGM by entering fingerprick data. Check your blood sugar at least 5-6 times a day and enter it into the system, and the bionic pancreas will know what to do and adjust accordingly. So you can take a break from the CGM to go to the beach for the weekend if you want, and the system will still know what to do. The bionic pancreas technology is smart, and it learns your insulin needs, and adjusts the insulin delivery accordingly over time.
2:34pm – Allows for a microburst of glucagon in the event that you want to do something cool like go swimming, and need to raise your blood sugar just a touch to accommodate for the increased activity level. Applies to other activities when you might want to disconnect your insulin pump as well. Like, “swimming.” With other people. When you don’t have anything to clip an insulin pump to. (Work with me here people!)
2:36pm – Now we’re learning the details of the Beacon Hill Study, which allowed participants of the study to traverse all over downtown Boston in a 3-mile area with a nurse in tow. The nurse was required for the study, just in case there were any problems (there weren’t, by the way).
Check out Kelly Close’s report on her experience as a participant in the Beacon Hill Study on diaTribe.
2:41pm – The average A1C of the participants of the study was 7.1. The bionic pancreas got their A1C even better, without the hypo (low BG) episodes. Incredible!

2:46pm – In the 2013 summer camp study, which was trialed with T1D adolescents, the bionic pancreas system provided an average BG of 159.
2:50pm – The Bionic Pancreas Multi-Center Study is an 11-day experiment with the bionic pancreas where the patients can wear the system home, without a nurse, and even drive and go to work like they would any other day. No one has ever driven with the bionic pancreas, so this will be a first in more ways than one.
Pivotal Study: Mid-2015-mid-2016 (will be patients wearing the pump for several months).
Review of PMA by FDA: Late 2016-mid-2017
Bionic Pancreas IS ON TRACK to be completed and FDA-approved by the time David (Ed’s son) goes to college.
For more information, visit the Bionic Pancreas on the web at www.bionicpancreas.org.
2:55pm – Now we’re going to hear from Scott Scolnick, who was a participant in the Beacon Hill Study. He was participant number B23, and this is his story about that experience.
Messages heard and learned along the way:
– There will be a cure in 10 years.
– I likely would not live to be 40.
– I could still ski.
– The looks and comments.
– Need to think/be aware about EVERYTHING that I DO and EAT.
Scott (and me) recommend the book “Diabetes Burnout” by Bill Polansky, Ph.D., CDE. Bill is one of my favorite people in the diabetes field, and deals with the mental and emotional impact of diabetes on the people who carry that burden day in and day out.
3:00pm – Scott is committed to living well with diabetes for himself, and also for his three daughters.
Scott is also an avid foodie. Check out his site InsulinWorthy.com to figure out if what you eat (in Boston, for now) is worth the insulin you have to take to cover it. I wish I had known about this site when I was in Cambridge last summer. Very cool!
Scott is a major Boston Red Sox fan. He has a dog named Fenway, and changes his glasses every time that the Red Sox lose. Major fan.
3:08pm – Scott participated in the Beacon Hill Study for 6 days/5 nights. His goal was to eat his way through Boston, and try to break the bionic pancreas and the algorithm. In his words, “There was no food that was safe from me. Nothing!”
After 24 hours of being on the bionic pancreas and eating 5 slices of pizza, Scott’s BG spiked to 202, and came down much faster than by manual bolusing (with pens or typical pump). Because the system was doing such a good job of learning Scott’s diabetes, it was able to adjust and predict based on his particular diabetes needs.
3:13pm – On Friday of the study, Scott told the nurse traversing around Boston with him that he didn’t want to know what his blood sugar was anymore. It was the most freeing feeling not having to know, and not having the burden, and not having to think about diabetes. It allowed him to enjoy everything else so much more.
(Note: There are tears rolling down faces in the conference right now. This story, and the idea of not having to carry the heavy burden of diabetes, and the technology being so close to a reality… It really feels like a dream coming true.)
3:20pm – On the drive home, after the Beacon Hill Study ended, reality set in. Now Scott had to go back to managing and making decisions about and being the control freak about his diabetes again, and it was a harsh reality to have to face after 6 days/5 nights of not having to worry about diabetes and make diabetes decisions at all. And it comes in waves, even still.
The bionic pancreas is real. Scott says if he couldn’t break it, then it is definitely real. And it’s coming. And I want it. Have I mentioned that?
3:30pm – Very excited to hear the beloved Joe Solowiejczyk talk next about his more than 54 years with diabetes. And something about diabetes and risky behaviors. Check out his website, www.amileinmyshoes.com.
3:40pm – “If you’re not doing risky behaviors, then you’re really not alive. The only thing that gets in the way of the risky behavior shit, is the diabetes shit.” I love Joe Solo. He’s the best, and tells it exactly like it is.
3:45pm – Discussing the most important reasons of why you take care of yourself. A lot of reasons being shared. What are the 3 reasons why you take care of yourself and your diabetes? (Feel free to sound off about any of this stuff in the comments. Go nuts!)

3:55pm – “A big thing about living with a chronic illness is to not try to fix it, but to figure out how to guide it and go with the flow.” – Joe Solo
4:00pm – Next question: What are the 3 most common reasons/things that make you NOT want to take care of yourself? What are the obstacles that get in your way? (Answers shared include: There is no finish line. I don’t want to be a slave to the machines.
4:10pm – Diabetes is… “You go to bed with a 92, you wake up with a 220. What the hell? Did I dream of eating pizza?!”
4:15pm – Joe Solo Day – Schedule your diabetes depression days. Call a friend and say, “Hey, on Tuesday between 9am and 5pm I’m going to have a diabetes day and feel sorry for myself, and I want you to call me every hour and tell me how courageous and inspirational I am and how much you look up to me, etc. etc.” Then go and buy 2 pints of Ben & Jerry’s ice cream, and 5 tragic movies that will make you cry. You really have to ham it up. Then eenie-meenie-minie-mo until you pick the ice cream that you want, and you start. About an hour in, the phone rings, and people start telling you how courageous and inspirational you are, and you tell them, “Hey, thank you, that’s great, but the movie just started, call me back in an hour and tell me more” and hang up. An hour later, the phone rings again, and it usually only takes a few phone calls to wrap up your diabetes depression day and you’re ready to go again.
4:30pm – Next: What are the 3 ways in which you check out from taking care of yourself with diabetes? (Lots of group discussion. We all do it, from time to time. You can’t be “on” with diabetes all the time, even if life with diabetes does demand it.)
4:50pm – Joe Solo wrapped up a very entertaining and encouraging talk. Next we are taking a group picture, and then dinner, and then pool party at 8pm. Probably the last you’ll hear from me today. See you tomorrow! (MW)
Sunday, June 8, 2014 – SWD2014 National Conference
Dinner with D-friends at The Pub (Irish restaurant in Tampa) last night, followed by a pool party and a really nice chat with my friends Scott and Emily (check out their company Pump Peelz), followed by great conversation and friends in the hotel common area. I need more nights of chatting up people with diabetes, and talking about things both D and non-D related. The people here at SWD2014 are truly some of the best people in Martin World, and if you’re here next year, they can be some of the best people in your world too. I cannot recommend this conference enough if you are a young adult with diabetes. This is a safe place, where people understand the burden of living with fingerpricks and multiclicks, and where they give you the strength. courage, hope, and support to keep going.
9:15am – Nicole Johnson is welcoming everyone to the closing day of SWD2014. A lot of tired faces at breakfast this morning from a late, late, late night of socializing and sharing stories and experiences. Next up to talk to us about Diabetes Advances is Dave Joffee, a pharmacist and diabetes educator.
9:20am – Richard Bernstein was an electrical engineer that figured out that you could count carbs, check your blood sugar, and dose your insulin accordingly. The ADA didn’t support this way of thinking initially, but came around to the realization that Dr. Bernstein was onto something after many years. Bernstein is a proponent for a low carb diet (but we know, your diabetes may vary (YDMV)). His book, Dr. Bernstein’s Diabetes Solution, is a bestseller for those wanting more info on low carb diet.
9:25am – Novo Nordisk has a professional cycling team of people who all have Type 1 diabetes. For more information on Team Novo Nordisk, founded by Phil Southerland, check them out at www.teamnovonordisk.com.
9:35am – Diabetes technology has gotten more and more advanced over the years. Real-time continuous glucose monitors, audible BG meters that yell your blood sugar level at you (okay, maybe that’s not EXACTLY how Dave said it…but still), and strips that require less and less blood compared to years prior. Technology is making living with diabetes better and better, but also more complicated because there are more and more data points and variables to take into consideration.
9:40am – With all of this technology, we get stuck in habits with our diabetes and don’t use it. Not all technology works the way it was intended (e.g., air pressure injector for insulin).
9:42am – “20% of people who get an insulin pump continue to use it after 1 year. 80% abandon it, or don’t use it exclusively,” says Dave Joffe. This is why getting coverage of diabetes technology by insurance is problematic. The insurance company’s return on investment is low because the technology is not used and results in the same costly hospital visits or complications. (MW: More than half of the people in this room have an insulin pump right now, and many of those (with and without pumps) have a CGM. Doesn’t seem like they are inclined to take it off and change their routine to one that doesn’t include the technology, which conflicts with what Dave reports. Maybe it was an insurance company that did that research.)
9:48am – We can have all the technology in the world to help us, but when insurance companies refuse to cover it, it isn’t helping us. Cool new technology is only helpful if we, people with diabetes, who live with this disease day in and day out, can get it. Insurance companies making access to the technology that we need prohibitive drives me bananas! Like mine is doing with my Dexcom sensors right now. I have to appeal every month to my insurance company and convince them that yes, I do still need CGM sensors. Stop making me prove it every single month! </rant>
9:55am – Checking out insulin pumps. Animas, Medtronic, OmniPod, Asanti Snap, T:Slim. It’s like diabetes show and tell in here. Nothing incredibly new though.
9:58am – The idea of the design of the T:Slim pump is that if the pump were to malfunction, it wouldn’t dose 300 units from the reservoir into you without you knowing it. It would be limited to dosing only a small amount of insulin upon malfunction. (Seriously, has this ever happened? Even once? Chime in if you know, and I’ll update the live blog accordingly, but just seems like a scare tactic to me.)
10:00am – Insurance companies are trying to push people on injections back to R and NPH insulin, especially those with Type 2 diabetes because their use of insulin is often sporadic, and doesn’t merit the cost of the faster-acting insulins (Novolog, Apidra). For-profit insurance thinking, also driving me bananas.

10:05am – The trend in fitness tracking is adding even more data to the equation. All of these data points give us more and more things to make decisions on. There is a balance between having enough and too much information, and each person (with diabetes or otherwise) is going to have a different threshold for what is considered sufficient info.
10:10am – There are so many fitness apps on the market for smartphones. Pick one that works for you, and stick with it. (MW: I use the Weight Watchers app…because I’m a fat kid like that right now. I can’t express how difficult it is for me to track what I eat at every single meal and between meals, especially while traveling and working. Some weeks I do better with it than others. I also like the GoMeals app, and the FitBit app (though my FitBit itself only worked properly for a few short months). What fitness or tracking apps do you use and like, and why?)
10:15am – Next we welcome Tye Manor back to the Students With Diabetes National Conference for the 2nd year in a row to give us Leadership Principles to Live By. Last year he spoke at the SWD Leadership Conference, and this year we are excited that he is here to share with all of us.
10:18am – To be effective consistently, you fake it until you make it.
10:19am – Tye Manor. Pronounced “main-or.” Not “manure.” His joke, not mine.

10:21am – The most effective leaders have to listen well. They listen to understand. They do not listen to respond. They listen to everybody: coworkers, customers, children, everyone.
10:28am – Limit the amount of distractions in your world. When someone comes to talk to you, put your phone down, close your laptop, pick up a pad and a pen and listen with your full attention. This is an effective way to get things right the first time, because you listen to understand, rather than just to respond and move on to the next thing.
10:29am – When talking and working with other people…
1. Let the speaker speak.
2. Let your attention show. Show them that you are comprehending what they are saying.
3. Take notes. Do not trust your memory. Your memory will let you down. “The weakest ink will outlast the strongest memory.” Or “Don’t just think it, ink it.”
4. Concentrate. Train yourself to stay in the now, and not let your mind go off in other directions.
5. Pay attention to all of the details.
6. Pause. Think about what the person you are talking to is saying. People won’t think you are dumb if you pause. They will realize that you are giving careful consideration to what they said and/or how you want to respond.
10:42am – Leadership: The “L” stands for “listening.” Listening is the hardest thing you have to do all day long.
10:43am – LEadership: The “E” stands for “energize.” Leaders energize and inspire the people around them. Your job to be an effectively leader is not to lead people to water, where it is up to them whether they want to drink or not. Your job is to make them thirsty.
10:46am – LEAdership: The “A” stands for “action.” If you’re going to be successful in life, you can’t wait for things to happen. You must take action.
Check out Tye Manor’s book “Forget Patience, Let’s Sell Something” (if you didn’t dash up to the room and grab a copy out of his hands during his presentation).
10:49am – Keep moving forward. At any rate, fast or slow, keep forward motion. Success is the realization of a worthy goal.
10:51am – LEADership: The “D” stands for “develop a purpose.” Purpose will keep you moving forward despite your circumstances.
10:58am – Courteous determination (pushing through the “no”) is how you get to your goals.
11:05am – Fear is instilled in us to create action. Fear was never instilled in us to create paralysis. Purpose will give you the strength to face any brutality that is going on in your life. Being interested in being successful is not enough; you have to be committed to being successful.
11:08am – LEADErship: The “E” stands for “enable.” Some of the biggest mistakes in the world make money (e.g., Post-It Notes…who comes up with glue that won’t stick to anything? And now it’s a billion dollar industry.) 3M, the company responsible for Post-Its, enables their scientists at least 30% of their time to tinker and create new things. Many of them are failures, but some of them are successful or contribute to success of other products as well.
11:11am – LEADERship: The “R” stands for “reach out and reach back.” Always contribute and give back to your community, no matter how you define “community.” That is what defines you, gives you passion, and helps you fulfill your purpose.
11:15am – LEADERShip: The “S” stands for “self control.” Self control is extremely important as a leader.
11:18am – Now we’re talking about pet peeves. People parking in handicap spaces who are not handicap, people who don’t use their blinkers when they change lanes, grammar mistakes, being late, people who drive slow in the passing lane on the highway (a lot of really frustrated drives in this room…sheesh!).
11:23am – Now on to courteous behaviors. Saying thank you, smiling back at people, when a stranger tells you that you look nice (and they aren’t a serial killer), when someone at the grocery store lets you cut line, says “bless you” when you sneeze.
11:28am – LEADERSHip: The “H” stands for “handle relations well.” Always assume positive intent. Make it automatic. Practice. For example, when someone speeds by you on the highway, assume that they are on their way to help someone, and hope that they get there in time and safely.
11:32am – There is very often more than one way to accomplish a goal. Don’t assume that there is only one way to do something. Expect a different perspective.
11:41am – LEADERSHIp: The “I” stands for “integrity.” Who are you when nobody else is watching? That should be the same person that you are in public.
11:42am – LEADERSIP: The “P” stands for “positive.” Everyone has something that they are wrestling with. It’s human nature for us to focus on everything that is going wrong in our lives, and when we do it is hard to see the positive aspects of our lives. A child comes home with 5 A’s and 1 C, and we focus on the C instead of the 5 A’s.
11:46am – Last year, Tye lost his wife to breast cancer. It was the hardest thing that he has ever had to deal with, losing his best friend. (You can hear a pin drop in this room. None of us knew.) He shares that he could focus on that loss, but instead chooses to be thankful for all of the things that he has in his his life that are positive: His children, his family, his work, his church, etc. Starting tomorrow, Tye is starting a grief ministry at his church, to help other people who are dealing with grief and how to get through it in their own lives.
And you can too!
11:50am – SWD2014 is coming to a close. Nicole Johnson, Miss America 1999, Dr. of Public Health, and Executive Director of Bringing Science Home and Students With Diabetes, is on stage to share her story with diabetes, and call everyone here with diabetes to action, and encourage them to take everything we have learned home.
11:51am – Why do we do this with Students With Diabetes, have a national conference, and get people together from all over the United States? Connection, education, motivation, inspiration, and action.
11:57am – Nicole was diagnosed with Type 1 diabetes when she was in college. She was told she couldn’t compete. She was told that she couldn’t have kids. She continues defy the odds and advice of what she can’t do with diabetes, and has made it her mission in life to help others who are living with diabetes. Along with her daughter, Ava, who is perfectly healthy and has as much fun being around people with diabetes as the rest of us.
12:03pm – The SWD Internship program applications will be due by December this year. This is an incredible opportunity for students with diabetes to get paid internships in the diabetes business.
12:05pm – Planning for next year’s conference starts next week. I will be there, and I hope you will be too. Until next year at SWD2015, from Tampa, Florida, thanks for joining me for the live blog for the past three days. Be well, and keep in touch!–MW




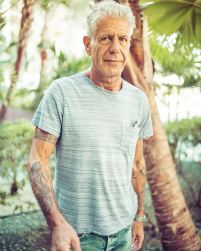 Recently we all lost Anthony Bourdain, and he was a master at asking very simple questions that allowed the people he interviewed to open up to him. I want my healthcare people to do the same with me. Sit down with me, away from the computer, and ask me very simple questions. How are you doing? What brings you in today? What is one thing I can do to help make your life better today? As Anthony Bourdain did with the people he met, ask me, directly and compassionately, what makes you happy?
Recently we all lost Anthony Bourdain, and he was a master at asking very simple questions that allowed the people he interviewed to open up to him. I want my healthcare people to do the same with me. Sit down with me, away from the computer, and ask me very simple questions. How are you doing? What brings you in today? What is one thing I can do to help make your life better today? As Anthony Bourdain did with the people he met, ask me, directly and compassionately, what makes you happy?